HAE is a rare genetic condition that causes repeated episodes or ‘attacks’ of severe swelling. HAE attacks can affect any part of the body, but the most commonly affected are the face, limbs and extremities, gut and airway.
Scientific advancements have unlocked significant progress in the treatment of HAE in recent years, with new therapies providing additional options for patients and clinicians, to manage the condition and reduce its impact on daily life.
However, some countries have been slower to adopt these new treatments than others, meaning that considerable variation exists internationally in patients’ access to treatment. Without action to remove barriers to access, there is a risk that progress will not be made on patient outcomes.
Takeda wants to be at the forefront of working with others to address these challenges. We therefore investigated variations in approaches to the management of HAE in Europe and Canada, to identify the extent to which patients in these countries are receiving care in line with international best practice standards
This site sets out some of the findings from our ‘Redefining Expectations’ report, which is aimed at supporting collaboration with patients, clinical experts and policymakers to drive improvements in outcomes for people living with HAE across the world.
Use the tabs at the top of the page to navigate the site.





In recent years, many countries have made progress in improving HAE outcomes. However, Takeda believes that more can be done to redefine expectations for HAE, across the patient journey.
We have identified four specific areas in which we believe progress can and should be made:
Too often people with HAE have to wait too long to receive a diagnosis. These delays can have a material impact on both their physical and mental wellbeing.
All health systems should set ambitious goals to reduce delays in diagnosis for HAE.
Patients with HAE have a diverse set of needs that require comprehensive support from a range of different health specialties.
There is a need for expert clinical and patient consensus to be forged on service standards and patient pathways, to inform the adoptions of best practice by health services.
There is a high level of international variation in access to treatments, with patients in some countries unable to access treatments recommended in international best practice guidelines.
Health systems should take steps to ensure that patients are able to access the medicines that are recommended by clinical experts and seek to provide rapid access to new treatments that could improve outcomes.
International collaboration between patient and clinical experts can be a key enabler of improved care. However, participation in international initiatives is not consistent.
National expert groups and networks should work with governments and healthcare systems to encourage greater collaboration in best practice sharing and data collection mechanisms.
Due to its rarity, the exact prevalence of HAE is still not known. Globally, it is thought to affect 1 in 50,000 people.1
The rarity of the condition creates significant challenges for people living with HAE, from diagnosis, through to treatment and care.
From the biological perspective, there are three main types of HAE:2
Early diagnosis of HAE is vitally important. Undiagnosed HAE is associated with poorer outcomes for patients, including a much higher risk of death.4
However, HAE is difficult to diagnose, as the symptoms are similar to those for many more common conditions. This can result in individuals seeing multiple healthcare professionals over an extended period of time before they are eventually diagnosed.
As a result, patients with HAE typically face long waits to receive a diagnosis, compared to those with more common conditions.
However, there are some signs that increased knowledge and understanding among clinicians is starting to drive down the average length of time patients have to wait in some countries, before receiving a diagnosis of HAE.5
Without effective treatment, some people living with HAE experience regular, lengthy and very painful attacks.
As a result, uncontrolled or poorly controlled HAE can have a significant impact on the ability of those affected to live normal lives, due to both the frequency and severity of attacks.
Scientific advancements have unlocked significant progress in the treatment of HAE in recent years, with new therapies providing additional options for patients and clinicians to manage the condition and reduce its impact on daily life.
However, some countries have been slower to adopt these new treatments than others, meaning that considerable variation exists internationally in patients’ access to treatment.1 Without action to remove barriers to access, there is a risk that progress will not be made on patient outcomes.
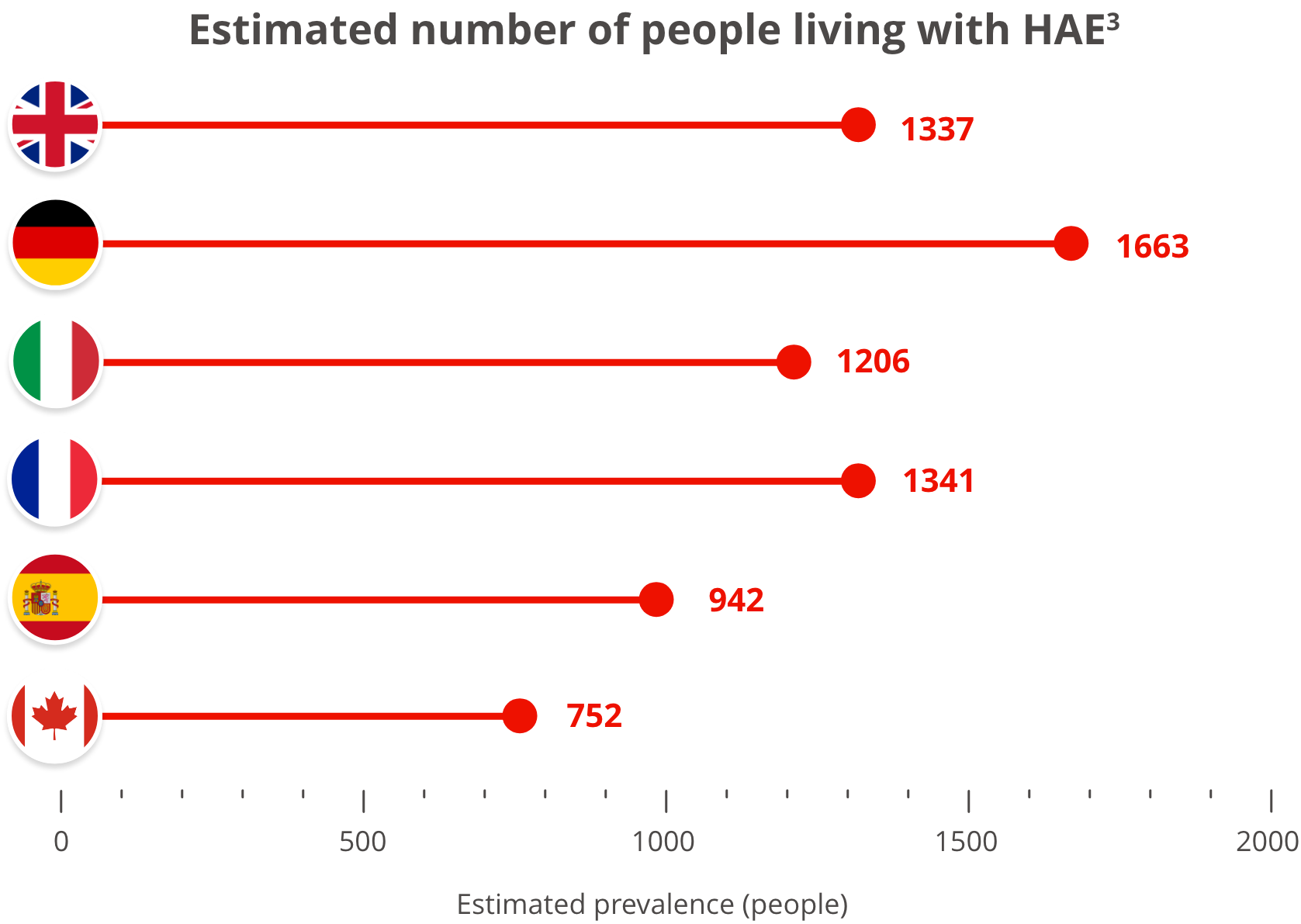
Use the map below to find out about the numbers of people living with HAE in Europe and Canada and click through to national patient organisation websites for more local information, resources and links.3
Total population:
Estimated people with HAE:
HAE patient organisation:
Source of population statistics (2019 data): https://data.worldbank.org/indicator/SP.POP.TOTL